.png?width=781&height=655&name=Untitled%20design%20(5).png)
Spinal compression fractures affect nearly one million people in the U.S. each year. They are most common in older people, especially women who are past menopause. Experts estimate that a quarter of women over fifty and nearly half of all people (including 40% of women) over eighty have experienced a spinal compression fracture.
What is a spinal compression fracture?
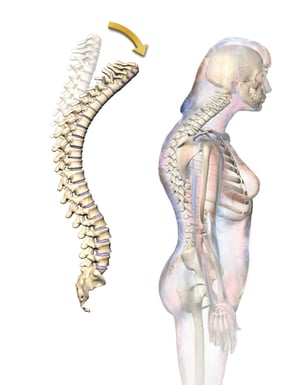
A compression fracture occurs when a vertebra develops a small crack or break, causing the spine to collapse. Most patients who suffer compression fractures have osteoporosis, in which the pores of the bones become larger, making the bones thinner and weaker. Over time, multiple vertebral fractures can cause an increase in the spinal curve, creating a hunched posture known as kyphosis.
What causes compression fractures?
In people with osteoporosis, the bones can become so weakened that compression fractures can result from everyday activities like sneezing, coughing, or other sudden spinal movement as well as from falls (particularly falls into a sitting position). In severe cases, simply bending forward can cause a compression fracture. In younger people and those without osteoporosis, auto and other types of accidents, severe falls, or the growth of tumors can cause compression fractures.
How do I know if I have a compression fracture?
In the beginning, people who gradually develop compression fractures may not experience symptoms. Sometimes, they’re discovered during imaging exams that are performed for other reasons. Over time, however, symptoms such as the following may develop:
- Back pain that increases gradually and may be relieved by lying flat
- Gradually decreasing height
- Decreased spinal mobility
- Incontinence
- Difficulty walking
- Numbness or tingling
- Kyphosis
When compression fractures occur due to sudden trauma, they often cause severe pain.
To diagnose a compression fracture, your doctor will look at your medical history and examine your spine. They will also likely order imaging exams such as X-ray, CT, or MRI to understand the precise location and extent of any fractures. A low-radiation bone density scan known as dual-energy X-ray absorptiometry (DEXA) may also be used to test for osteoporosis.
How are compression fractures treated?
In many cases, compression fractures heal on their own within two to three months, depending on their cause, and treatment typically includes rest, bracing, and pain medication. For patients with osteoporosis, medications may also be prescribed to help strengthen the bones. When fractures don’t heal following these treatments, doctors may recommend one of two minimally invasive procedures: vertebroplasty and kyphoplasty. Both procedures are performed under intravenous conscious sedation.
Vertebroplasty
After sedation is administered, an interventional radiologist makes a small incision in the patient’s back. The doctor then uses fluoroscopy, a type of moving X-ray image, to locate the fracture and use a needle to fill it with a special kind of cement. The cement mends the fracture and strengthens the spine. Most patients experience a reduction or elimination of pain within a few days, and some report immediate relief.
Kyphoplasty
Kyphoplasty is very similar to vertebroplasty. The difference is that before the bone cement is injected, a tiny balloon device is inserted into the fractured vertebra, creating a cavity. When the balloon is removed, the cement is injected in its place. Both procedures create a sort of internal cast that stabilizes the bone.
How can I reduce my risk of compression fractures?
While these spinal fractures are not always preventable, you can do several things to reduce your risk, such as
- Eat a healthy diet that includes ample sources of calcium and vitamin D.
- Avoid nicotine.
- If you drink alcohol, do so in moderation.
- Keep up on preventive health care visits.
- If you’re at risk for osteoporosis, consider a bone density test.
At Iowa Radiology, we want you to have all the information you need to make wise choices for your health. If you have questions about any of the procedures we perform, including vertebroplasty and kyphoplasty, please don’t hesitate to ask. To learn more about medical imaging and other important health care topics, feel free to browse our blog and our free resource library.
Resources
A Patient's Guide to Lumbar Compression Fracture. UMMS.org. Published 2003. Accessed April 12, 2022. https://www.umms.org/ummc/health-services/orthopedics/services/spine/patient-guides/lumbar-compression-fractures.
Compression Fracture. Cedars-Sinai.org. Published January 7, 2018. Accessed April 12, 2022. https://www.cedars-sinai.org/health-library/diseases-and-conditions/c/compression-fracture.html
Compression Fractures. ClevelandClinic.org. Published October 2, 2021. Accessed April 12, 2022. https://my.clevelandclinic.org/health/diseases/21950-compression-fractures.
Vertebroplasty & Kyphoplasty. Radiologyinfo.org. Reviewed March 23, 2021. Accessed April 12, 2022. https://www.radiologyinfo.org/en/info/vertebro


