New research emerges daily about the exciting new technology of breast tomosynthesis (better known as a “3-D mammogram.” Tomosynthesis provides a more complete picture of breast tissue by taking low-dose x-rays from many angles, yielding a truly three-dimensional image; this can improve a radiologist’s ability to identify abnormalities and improve detection and callback rates. Unfortunately, breast tomosynthesis still isn’t widely covered by insurance. Although Medicare began covering the exam on January 1, 2015, many private companies have not yet adopted this practice. How can you decide whether it’s right for you?
3-D vs. Traditional Mammogram
The answer may lie in the composition of your breasts. Recent studies indicate that for women with breasts considered “dense,” tomosynthesis significantly increased the cancer detection rate versus traditional two-dimensional mammography.[1] Only about 10% of women have breast tissue density considered "extremely dense," indicating a higher percentage of fibrous or glandular tissue vs. the percentage of fatty tissue.[2] Research has linked higher breast density with higher breast cancer risk, so increased vigilance in detection is even more vital in women with denser breasts.[3] In a Norwegian study of more than 25,000 women aged 50 to 69 with “dense” breasts, the detection rate of breast cancers increased from 59% to 80% when tomosynthesis was used in addition to traditional 2-D imaging.[4]
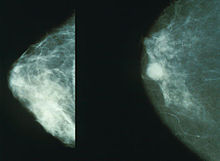
Getting the clearest picture possible is especially important for women with dense breasts, because both dense breast tissue and tumors appear white on traditional x-rays.[5] As a result, cancerous abnormalities can be missed. Also, many benign conditions appear on mammograms; dense tissue can more frequently appear to be suspicious, resulting in many costly (and frightening) additional tests, such as biopsies (surgical exploration to test the questionable tissue). Providers who have been using breast tomosynthesis in their practices since its origination report fewer false positives (suspicious tissue which turned out to be benign after further testing) and more instances of early detection using this technology than with traditional 2-D mammography.[6]
Regardless of the density of your breasts, another recently released study from the University of California San Francisco lends additional support to yearly radiographic screening beginning at age 40, even if you don’t have a strong family history of breast cancer.[7] For women whose breasts are considered “fatty,” which is common as women age, the same Norwegian study showed that 3-D mammography was still markedly superior at detecting cancer: 82% versus 63% detected by traditional mammography alone.[8] 3-D breast tomosynthesis technology can help ensure that your yearly screenings are as accurate as possible, which makes sense economically: early detection of cancerous abnormalities leads to more efficient, effective treatment options, and fewer false positives mean less unnecessary and potentially invasive follow-up testing, in addition to the priceless peace of mind that greater certainty affords.
Iowa Radiology offers breast tomosynthesis to our mammography patients for an additional charge of only $40 if your insurance doesn't cover it. The exam takes about the same time as a traditional mammogram.
To learn more about your mammogram options, download our ebook.
The information contained in the Iowa Radiology website is presented as public service information only. It is not intended to be nor is it a substitute for professional medical advice. You should always seek the advice of your physician or other qualified healthcare provider if you think you may have a medical problem before starting any new treatment, or if you have any questions regarding your medical condition.
Iowa Radiology occasionally supplies links to other web sites as a service to its readers and is not in any way responsible for information provided by other organizations.
Sources
[1] http://www.medscape.com/viewarticle/835900[2] Ibid.; http://www.sciencedaily.com/releases/2014/12/141202082411.htm
[3] http://www.sciencedaily.com/releases/2014/12/141202082411.htm
[4] http://www.medscape.com/viewarticle/835900
[5] http://www.medscape.com/viewarticle/835900
[6] http://pubs.rsna.org/doi/abs/10.1148/rg.344130087
[7] http://www.modernhealthcare.com/article/20141202/BLOG/312029995
[8] http://www.sciencedaily.com/releases/2014/12/141202082411.htm